Osteoporosis and declining bone health are serious health risks among perimenopausal and post menopausal women. Osteoporosis is characterized by declining bone strength and quality that predisposes women to increased risk of fractures, most commonly in the spine and hip.
Most women believe that their bones only start to weaken much later in life or post-menopausally, but the unfortunate reality is that the greatest amount of bone losses actually occur in the menopause transition (perimenopause).
Women experience an average bone loss of approximately 2% in the 1-3 years prior to menopause. Over the entire menopause transition (5-10 years), women will experience a 10-12% bone loss (approximately one T-score).
Why does this occur, and how do the hormonal changes that occur in the menopausal transition have such a significant impact on bone health?
In order to answer that question, you first have to understand the basics of our bone physiology and the important role of estrogen.
In adults, bone tissue is constantly undergoing change via the process of bone remodelling. This involves the removal of old bone by cells called osteoclasts, and replacement of new bone by osteoblasts (think B for “build”). Think of your skeleton as a house that is constantly under renovation. In younger women (<30 years old), there’s a balance between the demolition crew (osteoclasts) tearing down old walls and the construction crew (osteoblasts) building new ones. The house stays strong because every wall removed is quickly rebuilt.
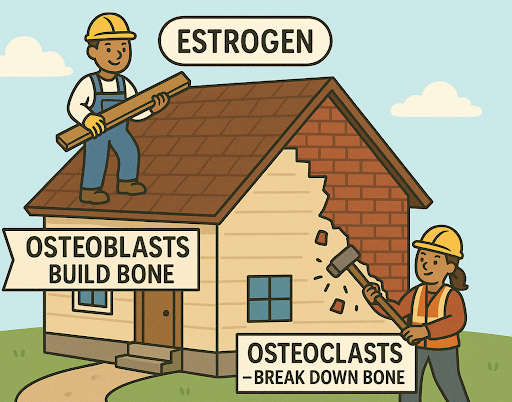
At menopause, estrogen—the “foreman” who keeps the teams balanced—steps away. Suddenly, the demolition crew starts working faster and harder, while the construction crew struggles to keep up. More walls are torn down than rebuilt, leaving the house weaker and less stable. Over time, this imbalance causes the framework (trabecular bone) and the outer walls (cortical bone) to deteriorate, much like a house that’s falling into disrepair.
Estrogen and Osteoporosis Prevention
Now that we know that estrogen plays a direct role in bone remodelling and positively influences the cells that build bone (osteoblasts), we can better understand how hormone therapy might help support bone health through the menopause transition.
How does using Estrogen and Menopausal Hormone therapy support bone health?
- Systemic hormone therapy containing estrogen can prevent bone loss in menopausal women and reduce fracture risk. Hormone therapy is indicated to prevent the occurrence of osteoporosis, not necessarily treat it. Once someone has osteoporosis, the strategy is to prevent further loss of bone density and reduce fracture risk. In the Women’s Health Initiative study (WHI), women receiving combined hormonal therapy treatment had a 34% reduction in vertebral and hip fracture risk.
- The impact that hormone therapy has on bone health is dependent on:
- Timing of Initiation: Hormone therapy is most efficacious and beneficial for bone health when initiated early in the menopause transition to help prevent the rapid bone turnover that occurs in the 1-3 years surrounding menopause.
- Dose of Estrogen: Higher doses of estrogen may have a greater benefit for supporting bone health in comparison to lower dose regimes.
- Duration of Use: The beneficial effects of estrogen on bone health will decline within a few months of stopping therapy. In these cases, women who choose to stop hormone therapy may decide to switch to another medication to prevent bone loss.
- Underlying Risk Factors: A lifetime of smoking, inactivity, medication overuse, poor diet or a genetic predisposition to osteoporosis unfortunately, cannot be solved with estrogen therapy.
Estrogen & Muscle Mass
Estrogen supports muscle health by binding to estrogen receptors that regulate genes involved in energy production, protein synthesis, and muscle repair. This helps maintain muscle mass, strength, and recovery capacity. Back to our house analogy: while our bones are the frame and foundation of the house, the muscles are the walls and support beams that help keep it stable. When estrogen levels fall after menopause, muscle metabolism slows, protein breakdown increases, and regeneration declines, leading to sarcopenia (muscle loss). Because bone and muscle “talk” to each other through shared hormones and cytokines, estrogen deficiency also weakens bones, raising the risk of osteoporosis.

As a menopause society certified practitioner and naturopathic doctor who works primarily with post menopausal women at risk of osteoporosis, I recommend taking a holistic approach to supporting your bone health. The first step is understanding your risk factors and getting a proper evaluation done to assess bone quality.
Emerging Therapeutics For Menopausal Women To Support Bone Health
Resveratrol: Resveratrol, a plant compound found in grapes and berries, can act like a weak estrogen and has shown benefits for circulation and bone health. In the RESHAW trial, postmenopausal women taking resveratrol (75 mg twice daily) for 12 months had improved bone density in the spine and hip, lower bone breakdown markers, and reduced fracture risk, especially when combined with vitamin D and calcium. These benefits were linked to better blood flow in bone tissue, suggesting resveratrol may help slow age-related bone loss.
Microbiome Modulation: The gut microbiome influences bone health by affecting nutrient absorption, immune balance, and gut-brain signalling. Microbes can protect against osteoporosis by reducing bone breakdown (osteoclast activity) and supporting bone-building cells (osteoblasts). While promising, more research is needed, though early clinical applications suggest gut microbes may aid in osteoporosis prevention.
Pyrroloquinoline Quinone (PQQ): Studies show that oxidative stress rises with age and contributes to postmenopausal osteoporosis. In an estrogen-deficient mouse model, supplementation with PQQ, a natural antioxidant, prevented bone loss and improved bone strength by reducing oxidative stress, slowing bone cell aging, and balancing bone formation and resorption. These effects were similar to estrogen treatment, suggesting PQQ may have potential to help prevent osteoporosis linked to low estrogen.

Conclusion
Menopause may bring big changes, but it doesn’t have to mean losing strength, resilience, or independence. By understanding how estrogen impacts your bones and muscles, you can take charge of your health during this transition. From exploring hormone therapy to embracing lifestyle strategies like movement, nutrition, and emerging natural supports, there are many ways to protect your foundation and feel stronger for years to come.
The most important step is knowing your risk factors and working with a knowledgeable practitioner to create a plan that fits your unique needs. Remember, your bones and muscles are living, dynamic tissues, and with the right support, you have the power to stay strong, vibrant, and confident well beyond menopause.
References
Geng Q, Gao H, Yang R, Guo K, Miao D. Pyrroloquinoline quinone prevents estrogen deficiency-induced osteoporosis by inhibiting oxidative stress and osteocyte senescence. Int J Biol Sci. 2019;15(1):58-68. doi:10.7150/ijbs.25783 pubmed.ncbi.nlm.nih.gov
Hsu B, Cumming RG, Blyth FM, et al. The impact of self‐reported arthritis on psychosocial health and quality of life: Findings from 45 and Up Study. Maturitas. 2020;136:64-71. doi:10.1016/j.maturitas.2020.04.009
International Menopause Society. Clinician’s Guide to Menopause Management. 6th ed. The North American Menopause Society; 2024.
Li JY, Yu M, Pal S, Tyagi AM, Dar HY, Wang J. The role of microbiota in osteoporosis and bone health. J Bone Miner Res. 2020;35(12):2172-2185. doi:10.1002/jbmr.4136
Meng J, Zhang Q, Pan J, et al. Regulation of skeletal muscle stem cell fate by estrogen and estrogen-related receptors. Maturitas. 2018;115:1-9. doi:10.1016/j.maturitas.2018.06.010
Ohlsson C, Vandenput L. Pharmacogenetics of osteoporosis: Focus on genome-wide association studies and gene–environment interactions. J Bone Miner Res. 2023;38(9):1743-1754. doi:10.1002/jbmr.4817
Resveratrol for Healthy Aging in Women (RESHAW): A randomized, double-blind, placebo-controlled crossover trial. J Bone Miner Res. 2020;35(11):2120-2131. doi:10.1002/jbmr.4135
Shang F, Zhang J, Wei M, et al. Exercise, bone health, and aging: The interaction between muscle and bone. Front Physiol. 2022;13:1078469. doi:10.3389/fphys.2022.1078469
Sun Y, Yu L, Wu J, et al. Estrogen receptor signaling and mitochondrial function in skeletal muscle. Int J Mol Sci. 2022;23(3):1376. doi:10.3390/ijms23031376
Zhang Y, Wang Y, Zhao J, et al. Emerging roles of bone-derived factors in energy metabolism regulation. Front Endocrinol (Lausanne). 2024;15:1273632. doi:10.3389/fendo.2024.1273632